Ever feel that uncomfortable burning sensation when you pee? Or have you found yourself rushing to the bathroom way more than usual. These could be signs of a urinary tract infection (UTI).
Although UTIs are uncommon, you should still pay attention to them. In this post, we’ll explain everything you need to know about them, from what causes them to how to spot the symptoms.
We’ll also explain why seeing a doctor is crucial to avoid nasty complications. So, if you’ve ever wondered what’s happening down there, keep reading.
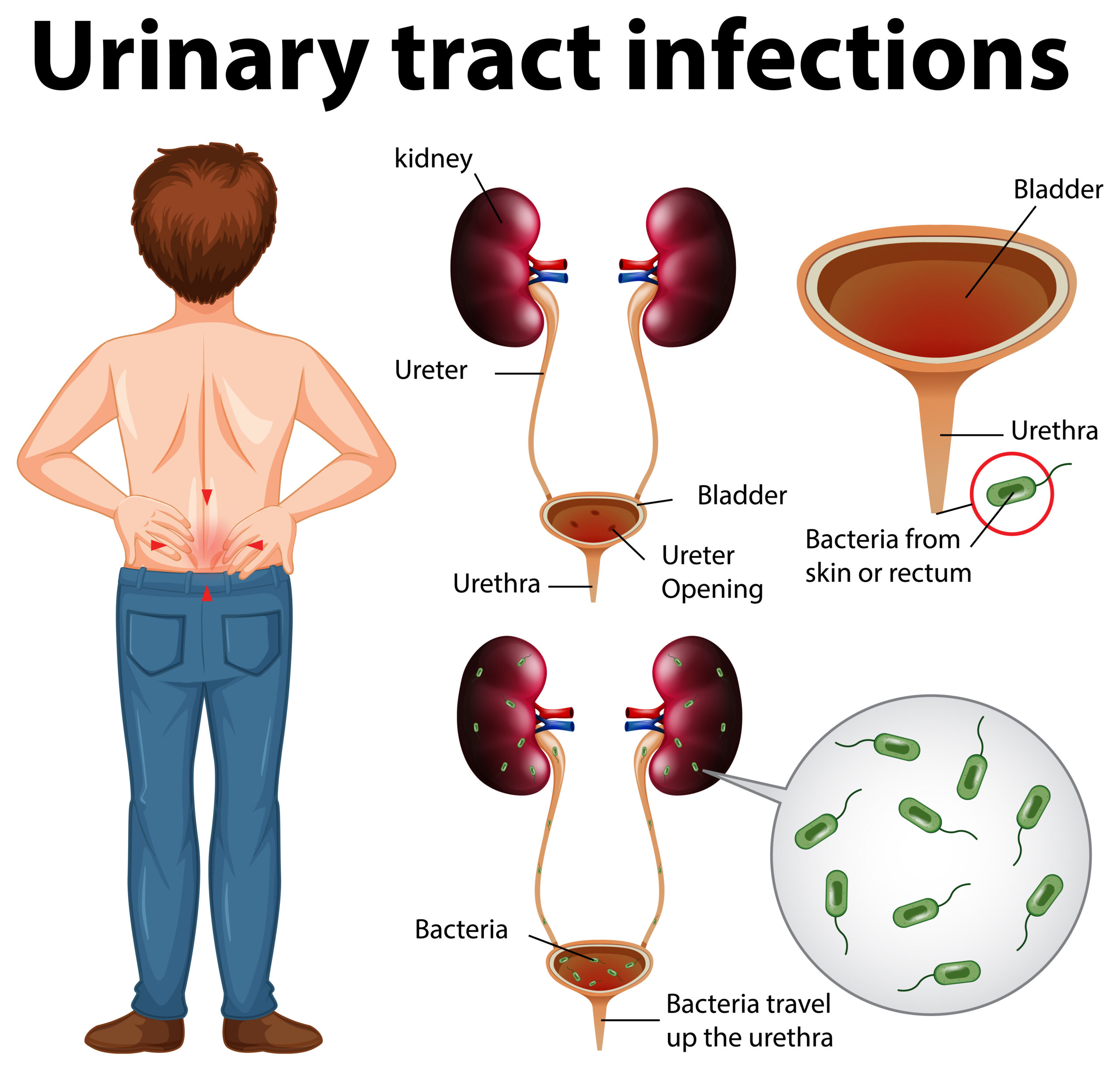
Understanding the Urinary System
The urinary system is often likened to the body’s drainage system. It plays a vital role in maintaining our overall health and well-being. Comprising a network of organs and structures, it is responsible for eliminating waste products and excess fluids from the body.
Understanding the division of the urinary system into the upper (kidneys and ureters) and lower (bladder and urethra) components is essential for comprehending the pathophysiology of urinary tract infections (UTIs).
Dysfunction or infection within any of these structures can disrupt the normal urine flow and lead to various urinary complications.
Let’s take a closer look at the components of this intricate system:
Kidneys
The kidneys are the urinary system’s filtration powerhouse in the upper abdominal area. They filter waste products, excess salts, and fluids from the blood, producing urine as a result. Additionally, the kidneys play an essential role in regulating blood pressure, electrolyte balance, and the production of red blood cells.
Ureters
Extending from each kidney, the ureters are slender tubes that transport urine from the kidneys to the bladder. These muscular tubes use peristaltic contractions to propel urine downward, ensuring a unidirectional flow toward the bladder.
Bladder
The bladder is a hollow, muscular organ in the pelvic cavity that acts as a temporary reservoir for urine. Its elastic walls expand and contract to accommodate varying volumes of urine, providing a sense of urinary control. The bladder’s sphincter muscles regulate urine flow into the urethra, preventing leakage between voiding.
Urethra
The urethra is a narrow tube that extends from the bladder to the external opening. It serves as the final pathway for urine excretion and, in males, as a conduit for semen during ejaculation. The length of the urethra differs between genders, with females typically having a shorter urethra than males.
Causes and Risk Factors of UTIs
Urinary tract infections (UTIs) are predominantly caused by bacterial invasion of the urinary system, particularly Escherichia coli (E. coli). However, other pathogens such as Klebsiella, Proteus, and Enterococcus can also be culprits. Understanding the factors contributing to the development of UTIs is crucial for prevention and treatment.
Bacterial Infections
The most common cause of UTIs is the introduction of bacteria into the urinary tract. E. coli, found in the gastrointestinal tract, is the primary offender, often entering the urethra and ascending to the bladder, leading to infection. Other bacteria can colonise the urinary tract through various mechanisms, triggering infection and inflammation.
Gender Differences
Due to anatomical differences, women are more susceptible to UTIs than men. The shorter length of the female urethra allows bacteria more access to the bladder, increasing the risk of infection. Additionally, hormonal changes during pregnancy and menopause can alter the urinary environment, making women more vulnerable to UTIs.
Urinary Stasis
Holding in urine for prolonged periods, commonly called urinary stasis, can promote bacterial growth and increase the risk of UTIs. Individuals who frequently delay urination, such as those with busy schedules or limited access to restroom facilities, are at higher risk. Urinary stasis allows bacteria to multiply within the bladder, leading to infection.
Sexual Activity
Sexual intercourse can introduce bacteria into the urinary tract, particularly in women. The friction and movement associated with intercourse can facilitate the transfer of bacteria from the perineal area to the urethra, increasing the risk of UTIs.
Additionally, specific contraceptive methods, such as diaphragms and spermicides, may further elevate the risk of infection.
Medical Conditions
Certain underlying medical conditions can predispose individuals to UTIs. Diabetes mellitus, for example, can impair immune function and promote bacterial growth in the urinary tract. Conditions that affect bladder function, such as neurogenic bladder and urinary retention, can also increase the likelihood of UTIs.
Dehydration
Inadequate fluid intake can concentrate urine and diminish urinary flow, creating an environment conducive to bacterial proliferation. Individuals who do not drink enough fluids may have reduced urinary output, allowing bacteria to remain in the urinary tract longer and increasing the risk of infection.
Pregnancy
Pregnancy imposes physiological changes on the urinary system, including increased urinary stasis and hormonal fluctuations, which can predispose pregnant individuals to UTIs. The growing uterus can exert pressure on the bladder, impairing complete bladder emptying and promoting bacterial growth.
Recent Medical Procedures
Specific medical interventions, such as urinary catheterization and urological surgeries, can introduce bacteria into the urinary tract and disrupt normal urinary function. Individuals who undergo such procedures may be at increased risk of developing UTIs, particularly if proper sterile techniques are not followed.
Signs and Symptoms of UTIs
Urinary tract infections (UTIs) can manifest with symptoms ranging from mild discomfort to severe complications. Recognizing the signs and symptoms of UTIs is crucial for prompt diagnosis and treatment. Here are the key indicators to be aware of:
Painful Urination (Dysuria)
One of the hallmark symptoms of a UTI is pain or burning sensation during urination. This discomfort is often described as a stinging or burning sensation in the urethra or bladder region. The intensity of pain can vary, ranging from mild discomfort to severe pain.
Increased Frequency of Urination
Individuals with UTIs may experience a heightened urge to urinate, coupled with increased frequency. They may make more frequent trips to the bathroom than usual, often passing small amounts of urine each time. This symptom is indicative of irritation and inflammation in the urinary tract.
Urgency to Urinate
Alongside increased frequency, UTI sufferers may also experience a sense of urgency to urinate. The sensation of needing to urinate may be sudden and intense, with little warning. Despite the urgency, individuals may find it challenging to empty their bladder, leading to incomplete voiding.
Nocturia
Nocturia refers to the frequent need to urinate during the night, disrupting standard sleep patterns. Individuals with UTIs may find themselves waking up multiple times during the night to urinate, even if they typically do not experience nocturia. This symptom can significantly impact sleep quality and overall well-being.
Cloudy or Bloody Urine
UTIs can change the appearance of urine, making it cloudy, murky, or discoloured. In some cases, urine may contain visible traces of blood, indicating inflammation or infection within the urinary tract. Bloody urine, known as hematuria, warrants prompt medical attention.
Foul-Smelling Urine
UTIs can produce urine with a strong, unpleasant odour, often described as foul-smelling or pungent. The odour may be noticeable even from a distance and typically indicates bacterial overgrowth in the urinary tract.
Pelvic Pain or Discomfort
In addition to urinary symptoms, some individuals with UTIs may experience pelvic pain or discomfort. This pain can manifest as a dull ache or pressure in the lower abdomen or pelvic region and may worsen during urination.
Systemic Symptoms
In severe cases, or if the infection spreads to the kidneys, individuals may experience systemic symptoms such as fever, chills, nausea, and vomiting. These symptoms suggest a more severe disease and require immediate medical attention.
Risks and Complications of UTIs
While urinary tract infections (UTIs) are often considered common and relatively minor, they can lead to severe complications if left untreated. Understanding the potential risks and complications associated with UTIs is crucial for prompt intervention and prevention of long-term health issues. Let’s look at some of the possible risks and complications:
Kidney Infection (Pyelonephritis)
One of the most severe complications of untreated UTIs is the potential spread of infection to the kidneys, resulting in pyelonephritis. In pyelonephritis, bacteria ascend from the bladder or ureters into the kidneys, leading to inflammation and infection of the renal tissue.
This condition can cause severe pain in the back or side, high fever, chills, nausea, and vomiting. Pyelonephritis requires immediate medical attention and may lead to kidney damage if left untreated.
Sepsis
In severe cases, untreated UTIs can lead to sepsis, a life-threatening condition characterised by a systemic inflammatory response to infection. Sepsis occurs when the body’s immune system overreacts to the presence of bacteria, causing widespread inflammation and organ dysfunction.
Symptoms of sepsis include high fever, rapid heart rate, rapid breathing, confusion, and decreased urine output. Sepsis requires urgent medical intervention and can be fatal if not treated promptly.
Recurrent Infections
Individuals who experience frequent or recurrent UTIs are at risk of developing complications over time. Recurrent UTIs can lead to chronic inflammation of the bladder and urethra, increasing the likelihood of antibiotic resistance and complicating treatment.
Moreover, repeated episodes of infection may predispose individuals to kidney damage and other urinary tract abnormalities.
Chronic Kidney Disease
Prolonged or recurrent kidney infections can cause damage to the kidneys over time, leading to chronic kidney disease (CKD). CKD is a progressive condition characterised by the gradual loss of kidney function, which can eventually result in kidney failure.
Individuals with CKD may experience symptoms such as fatigue, fluid retention, high blood pressure, and electrolyte imbalances. Management of CKD typically involves lifestyle modifications, medication, and, in advanced cases, dialysis or kidney transplantation.
Pregnancy Complications
Untreated UTIs during pregnancy can pose risks to both the mother and the developing foetus. In addition to increasing the risk of kidney infections, untreated UTIs during pregnancy can lead to preterm birth, low birth weight, and other complications for the baby.
Pregnant individuals with UTI symptoms should seek prompt medical evaluation and treatment to minimise the risk of adverse outcomes.
Chronic Pelvic Pain
Some individuals may develop chronic pelvic pain syndrome as a result of recurrent UTIs or unresolved urinary symptoms. Chronic pelvic pain can significantly impact quality of life and may require multidisciplinary management approaches, including medication, physical therapy, and psychological support.
Treatment of UTIs
Effective treatment of urinary tract infections (UTIs) involves a combination of medical intervention, lifestyle modifications, and preventive measures. Prompt diagnosis and appropriate management are essential to alleviate symptoms, prevent complications, and eradicate the underlying infection.
Here’s an overview of the primary components of UTI treatment:
Medical Evaluation
Upon experiencing symptoms suggestive of a UTI, seeking medical evaluation from a healthcare provider is crucial. The diagnosis of UTIs typically involves a thorough medical history review, physical examination, and laboratory tests, such as urinalysis and urine culture.
These tests help confirm the presence of bacteria in the urine and identify the specific type of bacteria causing the infection.
Antibiotic Therapy
The cornerstone of UTI treatment is antibiotic therapy, which aims to eradicate the bacterial infection. Antibiotics prescribed for UTIs target the specific bacteria responsible for the infection, with common options including trimethoprim-sulfamethoxazole, nitrofurantoin, ciprofloxacin, and amoxicillin-clavulanate.
The choice of antibiotic depends on factors such as the severity of symptoms, bacterial susceptibility patterns, and individual patient characteristics. It’s essential to complete the entire course of antibiotics as the healthcare provider prescribes, even if symptoms improve before completing the treatment.
Symptomatic Relief
In addition to antibiotics, symptomatic relief measures may be recommended to alleviate discomfort associated with UTI symptoms. Over-the-counter pain relievers such as ibuprofen or acetaminophen can help relieve pain and reduce fever.
Additionally, drinking plenty of fluids, particularly water, can help flush out bacteria from the urinary tract and promote healing.
Follow-Up Evaluation
Following the completion of antibiotic therapy, a follow-up evaluation may be recommended to ensure the resolution of the infection and assess for any lingering symptoms or complications. In some cases, repeat urine testing may be performed to confirm the eradication of bacteria from the urinary tract.
Individuals with recurrent UTIs or persistent symptoms may require further evaluation and management by a healthcare provider.
Management of Underlying Conditions
Individuals with underlying medical conditions such as diabetes or urinary tract abnormalities may require additional management to reduce the risk of recurrent UTIs. Optimising control of underlying medical conditions and addressing predisposing factors can help minimise the likelihood of future infections.
Preventive Measures
Preventive measures and lifestyle modifications may be recommended to reduce the risk of recurrent UTIs. These may include:
- Drink plenty of water to maintain adequate hydration and promote urinary flow.
- Urinate frequently and empty the bladder to prevent urinary stasis and bacterial growth.
- To prevent the spread of bacteria, practice good hygiene, including wiping from front to back after using the bathroom.
- Avoid irritants such as bubble baths, harsh soaps, and feminine hygiene products that may disrupt the natural balance of bacteria in the urinary tract.
- Urinating before and after sexual intercourse to help flush out bacteria from the urethra.
- Prophylactic antibiotic therapy should be considered in select individuals with recurrent UTIs or specific risk factors.
Wrapping Up
Urinary tract infections (UTIs) are common yet significant health concerns that can impact individuals of all ages and genders. In this blog, we’ve emphasised the importance of prompt diagnosis, appropriate treatment, and effective preventive measures in managing UTIs.
By seeking medical evaluation, adhering to antibiotic therapy, and implementing lifestyle modifications, individuals can alleviate symptoms, prevent complications, and reduce the risk of recurrent infections.